Top Eye Symptoms of COVID-19 (Coronavirus Disease)
The eyes have been described as the “window to the soul” but they may also be a window into the coronavirus disease 2019 or COVID-19 as we’ve come to know it—especially as scientists learn more about the short-term and long-term ocular effects.
Prevalence of COVID-19 Eye Symptoms
By now, the medical community and general population have developed a solid understanding of the core symptoms of COVID-19: fever, dry cough, shortness of breath or difficulty breathing, and loss of taste or smell, among others. Although these issues dominate the majority of confirmed coronavirus infections, the eyes have become an increasing focus among scientists looking for additional signs and symptoms of the disease.
In fact, it is estimated that between 10-30% of COVID-positive patients can experience ocular complications, although some studies have suggested that perhaps as many as 70 percent have at least one eye-related symptom.1-3 Other evidence has even shown that certain eye problems may be the earliest indicators of COVID-19 infection, appearing before general respiratory complaints and/or fever.
Top Eye Symptoms
Caused by COVID-19 Infection

It is important to distinguish between those symptoms that are believed to be caused by the coronavirus disease and those that may co-occur with the infection but have a secondary cause (e.g. such as those stemming from environmental influences). Although to be clear, there is significant overlap in these symptoms—which makes it hard to know exactly what the root cause may be.
These are the leading ocular symptoms of COVID-19:1-4
|
Top COVID-19 Eye Symptoms as reported by patients |
|
| Burning sensations | 10-36% |
| Epiphora (Watery Eyes), Tearing | 12-32% |
| Ocular Discharge | 4-30% |
| Itchiness, Redness | 11-24% |
| Photophobia | 11-20% |
| Sore Eyes | 16% |
| Eye Pain | 10-18% |
| Foreign Body Sensation | 4-19% |
Generally, scientists have connected these symptoms directly to the viral infection. In particular, the coronavirus infiltrates the membrane surrounding the whites of your eye and extending beneath the eyelid. This leads to conjunctivitis (which we know as “pink eye”), thus triggering the numerous effects described above. It is certainly possible that other mechanisms are involved in the onset of these symptoms, but conjunctivitis is believed to be the main cause.
How does COVID-19 penetrate the eye?
This is the million dollar question: how does the virus get into our eye in the first place? Several explanations have emerged from medical professionals. First, hand-to-eye contact (whether it is frequent or infrequent) has been linked to higher likelihood of conjunctivitis and eye-specific symptoms.4 This reinforces why hand washing continues to be a critical measure for individuals to protect themselves against the coronavirus.
In addition, patients can be exposed through viral particles in the air. According to Harvard Health, the coronavirus can remain in the air for up to 3 hours, which naturally increases the risk that we may breathe in these particles or otherwise have them penetrate through our eyes. Certainly, the type of environment—for example, a confined, poorly-ventilated space versus an open air location—can play a significant role in exposure too. Some researchers have even found that wearing eyewear like regular glasses or protective goggles could potentially reduce the risk for infection, but more substantive research is needed.5,6 Still, mask wearing and physical distancing remain the most effective strategies for self protection.
Other Eye Symptoms
Associated with COVID-19
There is notable discrepancy in the number of ocular complaints from patients (as high as 70% in some studies) and confirmed cases of conjunctivitis (usually 11% or lower), so there must be other causes for eye symptoms!7,8 The following have been cited by COVID-positive patients in the absence of conjunctivitis:
- Dry eyes
- Blurred vision
- Photophobia
- Eye pain
- Eye tearing, epiphora
- Ocular itchiness, redness
- Visual floaters or flashes
- Foreign body sensation
So what causes them? A whole host of potential underlying reasons for these complications have been identified, although much uncertainty remains. One purported reason is the development of other primary symptoms during the infectious period, such as headache. On average 10-30% of patients develop recurring and/or severe headaches as a result of the coronavirus, and these headaches can have migraine-like features—which includes photophobia, blurry vision, and dry eyes, among other possible ocular concerns.
Another possible cause may not have anything to do with the infection itself, but other changes that impact the patient. For example, one study found that dry eyes and blurry vision were among the most common ocular manifestations of COVID-19, but they theorized that patients often self isolate as a result of their positive test (whether at home or under medical care); this leads to an increased use of electronic devices, which in turn exposes them to artificial blue light and bright light—both of which can lead to the eye symptoms they experience. We know that the pandemic has likely, and substantially, increased screen exposure for most individuals, so it is no surprise that coronavirus patients would also experience similar consequences.
Additionally, pre-existing conditions can negatively influence the symptoms and outcomes of acute COVID infection. The medical community is only beginning to scratch the surface of exactly what other disorders affect patient experiences and the unique medical care they may require; neurological issues (e.g. migraine or traumatic brain injury), certain types of cancer and underlying ocular disease may worsen eye-related symptoms if introduced to viral infections like COVID-19.
Duration of Ocular Symptoms
COVID-19 problems affecting the eye do not appear to develop abnormally, with most appearing around the time of systemic symptoms (fever, respiratory). The vast majority manifest within one week of other symptoms, although some reports have suggested that a smaller subset of patients can develop ocular complications several weeks before OR after the core symptoms.1,9
While each case of COVID-19 infection is different, recent studies have indicated that the majority (around 80%) last between one to two weeks, usually following the course of the general recovery process.1 Other studies have shown that maybe one in four people will have symptoms beyond the resolution of the infection, even when no virus can be detected in the body—with some lasting even months later.9
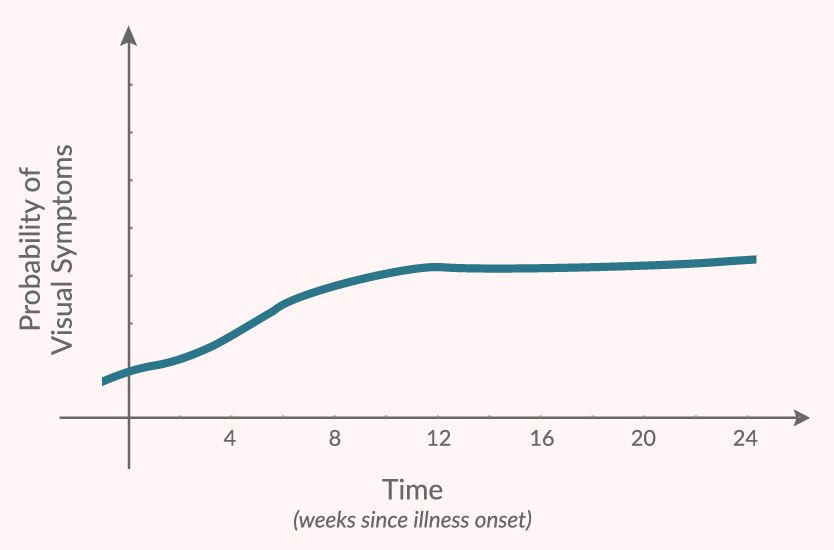
Patient data shows that eye-related symptoms often become more likely in the weeks following infection (source)
A comprehensive survey—which explored the symptoms of patients up to 7 months post infection—highlighted that many visual symptoms associated with the coronavirus disease tend to follow a similar path. While they occur before and during the infectious phase, they actually increase in prevalence immediately following the acute infection before peaking after approximately one month. Although the risk for symptom onset stabilizes at that time, they still tend to remain an ongoing problem.10
It is unclear the extent to which these COVID “long haulers,” as they are sometimes called, will impact people in the months and years following their diagnosis. And again, we are only beginning to learn about the longer-term effects of COVID-19 on our bodies, which will take years to fully understand.
Risk Factors for Eye Problems
As previously mentioned, eye exposure to infectious COVID-19 particles—either through the environment, lack of proper eye protection and/or hand-to-eye touch—has been associated with increased likelihood of ocular symptoms. However, researchers have noted some other potential complicating factors of which to be aware, specifically:11
- Higher fever
- Older age
- Pre-existing eye condition
There is also evidence that eye-related symptoms are indicative of a more serious disease progression with coronavirus, although that may more likely result from other high-risk complications.12 We expect that scientists will continue to keep close watch on these effects and make further recommendations for patients both during and after infection.
References:
1Pardhan S, Vaughan M, Zhang J, Smith L, Chichger H. Sore eyes as the most significant ocular symptom experienced by people with COVID-19: a comparison between pre-COVID-19 and during COVID-19 states. BMJ Open Ophthalmology. 2020;5(1). doi:10.1136/bmjophth-2020-000632.
2Aggarwal K, Agarwal A, Jaiswal N, et al. Ocular surface manifestations of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Plos One. 2020;15(11). doi:10.1371/journal.pone.0241661.
3Rokohl AC, Loreck N, Matos PAW, et al. More than loss of taste and smell: burning watering eyes in coronavirus disease 2019. Clinical Microbiology and Infection. 2020;26(11). doi:10.1016/j.cmi.2020.08.018.
4Chen L, Deng C, Chen X, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID‐19 in Wuhan, China: a cross‐sectional study. Acta Ophthalmologica. 2020;98(8). doi:10.1111/aos.14472.
5Maragakis LL. Eye Protection and the Risk of Coronavirus Disease 2019. JAMA Ophthalmology. 2020;138(11):1199. doi:10.1001/jamaophthalmol.2020.3909.
6Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. The Lancet. 2020;395(10242):1973-1987. doi:10.1016/s0140-6736(20)31142-9.
7Güemes-Villahoz N, Burgos-Blasco B, García-Feijoó J, et al. Conjunctivitis in COVID-19 patients: frequency and clinical presentation. Graefe's Archive for Clinical and Experimental Ophthalmology. 2020;258(11):2501-2507. doi:10.1007/s00417-020-04916-0.
8Loffredo L, Pacella F, Pacella E, Tiscione G, Oliva A, Violi F. Conjunctivitis and COVID‐19: A meta‐analysis. Journal of Medical Virology. 2020;92(9):1413-1414. doi:10.1002/jmv.25938.
9Gangaputra SS, Patel SN. Ocular Symptoms among Nonhospitalized Patients Who Underwent COVID-19 Testing. Ophthalmology. 2020;127(10):1425-1427. doi:10.1016/j.ophtha.2020.06.037
10Davis HE, Assaf GS, Mccorkell L, et al. Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. 2020. doi:10.1101/2020.12.24.20248802.
11Bostanci Ceran B, Ozates S. Ocular manifestations of coronavirus disease 2019. Graefes Arch Clin Exp Ophthalmol. 2020;258(9):1959-1963. doi:10.1007/s00417-020-04777-7
12Nora RLD, Putera I, Khalisha DF, Septiana I, Ridwan AS, Sitompul R. Are eyes the windows to COVID-19? Systematic review and meta-analysis. BMJ Open Ophthalmology. 2020;5(1). doi:10.1136/bmjophth-2020-000563.
TheraSpecs Glasses for Light Management
Try our light-filtering glasses and stay protected against harsh light from screens, fluorescents, LEDs, unwanted blue light, bright sunlight, flashing lights, and more.





