Is the COVID-19 Pandemic Causing More Screen-Related Headaches and Migraine Attacks?
It’s safe to say that most of us are feeling the effects of the COVID-19 (coronavirus) pandemic, in one way or another. From disruptions in our daily activities or our work lives to noticeable impact on our physical and mental health, this has been a game changer. And for many with chronic illness—particularly those with neurological conditions that cause headaches, light sensitivity and other symptoms—these dramatic and abrupt changes have taken their toll.
At TheraSpecs, we wanted to better understand how the pandemic, “stay-at-home” orders and other lifestyle adjustments have influenced people’s screen time—and ultimately, whether that has led to any change in their symptoms. We gathered insights from online search trends and direct patient feedback as well as expertise from leading medical professionals, and they all helped us answer the question of whether or not people are experiencing more headaches and migraine attacks during this time. Here is what we found.
Screen time is going up
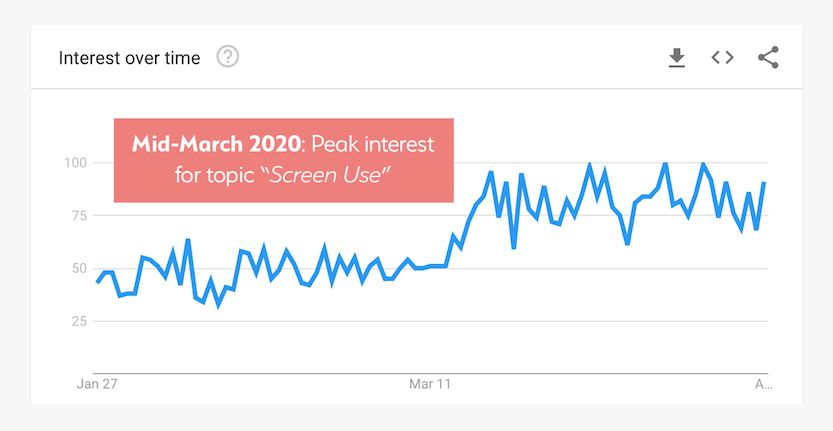
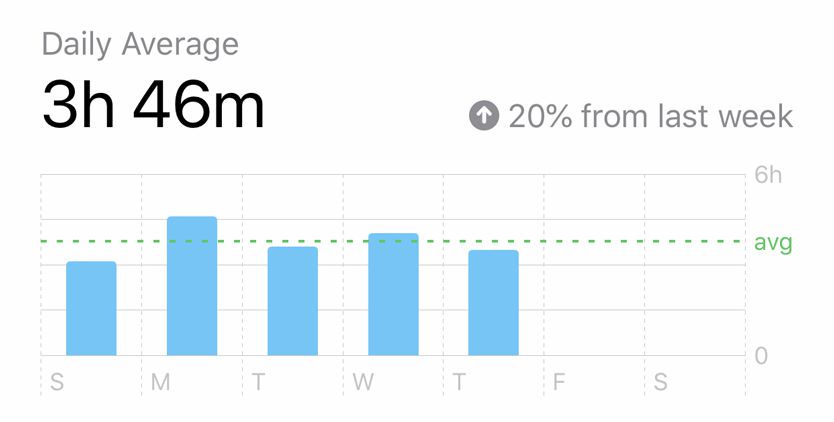
While verifiable evidence has been hard to come by, all signs point to a noticeable, and even significant, increase in screen time as a result of the COVID-19 outbreak. According to Google trends, the general interest in and searches related to the topic of “screen use” peaked in mid-March and has remained steady since then.
This is consistent with a recent report from the tech giant on broader consumer search trends, which highlighted clusters of new behaviors emerging during the pandemic. Their findings revealed that people were focusing on adjusting to changes in their routines and general self care. At minimum, this suggests that more people today are acutely aware of their exposure to device screens and broader concerns for their self-managed care.
In addition, a Global Web Index report found that 80% of U.S. and U.K. consumers are seeking out more content since the beginning of the pandemic, which likely translates to more time in front of a screen. And there has been particular emphasis on children’s screen usage as well, with one report showing that kid-focused digital apps have seen a 70% increase in visits and an overall 50% surge in daily screen hours for children.
But what about people with neurological conditions, like those with migraine or a traumatic brain injury (TBI)?
This is an area that hits home for all of us here at TheraSpecs, given our desire to improve the lives of individuals with light sensitivity. So we conducted an email survey of 338 people (260 of which self identified as being diagnosed with a neurological disorder) and came to similar conclusions. In fact, 78% of respondents believed that they have personally spent more time on their digital devices during the coronavirus crisis. Moreover, nearly two-thirds estimated that they were experiencing an increase of 3+ hours more per day of screen-related exposure.
We spoke with Dr. Joshua Tobin, neurologist and certified headache specialist at 21st Century Neurology in Phoenix, Arizona, and he confirmed that several of his migraine patients are seeing a rise in their screen use.
"About two-thirds of [the patients I’ve spoken with recently] have increased their screen time,” he said. “They’re working from home, they’re spending more time at the computer, more time videoconferencing, and that’s when the light sensitivity is a bigger issue."
As with Dr. Tobin's patients, the breakdown of digital activities is similar for our survey respondents:
- Connecting with friends or family (64%)
- Working from home (56%)
- Watching movies, television or streaming content (55%)
- Using social media (52%)
- Consuming online news (48%)
Telemedicine is also reshaping our exposure to digital devices. There have been reports of massive surges in virtual doctor appointments in light of COVID-19, including for centers that treat patients with neurological disorders. The New York Headache Center is one such organization that has largely migrated to video consultations for new patients and limited in-office visits, according to a website statement. We heard from other headache specialists, physical therapists and neurologists who told us the same about their practices.
All of this puts people with sensory sensitivities at greater risk for the onset or worsening of their symptoms; and that is exactly what we are seeing as a result.
More headaches, migraines and other symptoms too
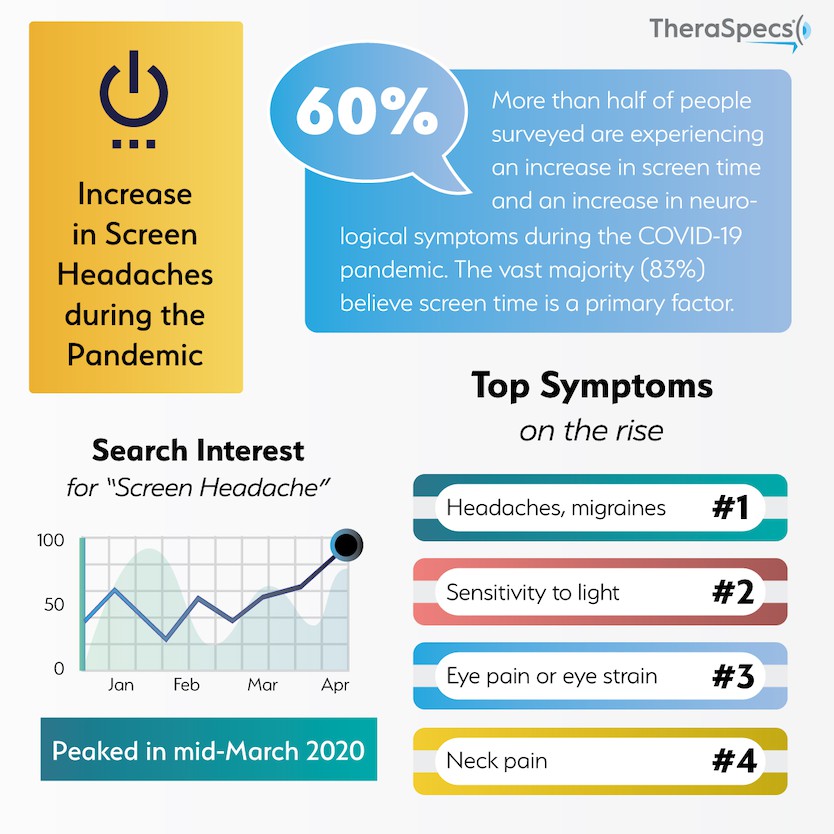
It appears there is a correlation between an increase in screen use and greater frequency of complications like headaches and migraine attacks. Our survey showed that nearly 60% of people who reported a rise in screen time also had more physiological side effects, with the greatest risk among those with the highest increases in daily exposure. Conversely, two-thirds of people with no change in regular screen exposure have similarly reported no change in their overall symptom load during the pandemic. While this does not conclusively prove that screens are a cause, the vast majority (83%) of people believed that it has at least contributed to the change in their health.
Dr. Tobin is seeing similar outcomes with his patients. "I’ve been asking patients if light is a trigger, and about 80% of them—which was a surprisingly high number to me—said yes. If these patients are also spending more time in front of a screen, they also tell me that their headaches are worse."
Stress, sleep disruption and other factors cannot be overlooked either. Headache and vascular disorder specialist Dr. Huma Sheikh of NY Neurology Medicine spoke with us about her direct interactions with patients experiencing a change in their symptoms.
"What I am hearing is a mixed bag, some feel somewhat better, likely due to less commute times...but others notice that the headaches are still occurring due to the stress of everything going on and being at home with kids a lot more," she said.
And what are the common symptoms people are experiencing? Our survey respondents represent a multitude of chronic conditions ranging from vestibular migraine and post-concussion syndrome to blepharospasm and lyme disease, so the complications are not just limited to headaches. These were the symptoms reported as having an increase in regularity:
- Headaches and migraine attacks (82%)
- Light sensitivity or photophobia (73%)
- Eye pain or eye strain (66%)
- Neck pain (66%)
- Dizziness or vertigo (43%)
- Blurred vision (35%)
While people with neurological disorders may be at greater risk, there is mounting evidence that people without these deficits are also having trouble adjusting to the new daily norms brought on by the pandemic. There was a spike in online searches in mid-March for “screen headache” and related phrases in Google, more than at any other time in the past 12 months. This trend has continued into April as well, indicating that these issues are not simply going away—although people may be developing consistent routines as well as taking additional steps to mitigate their screen use.

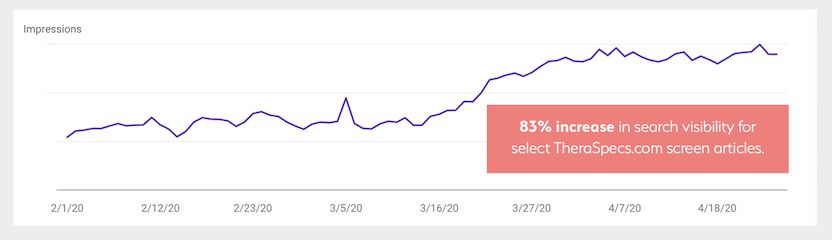
We have also seen a massive rise in online searches and visits to specific articles on the TheraSpecs website related to screen sensitivities. One of the most popular articles over the last few weeks and months is titled "Here’s Why Smartphones Can Hurt Our Eyes and Cause Headaches," which has been seen in hundreds of thousands of searches (an increase of 83%) and has more than doubled the number of views since March 15th.
We’re seeing similar gains for articles that focus on computer screen use, artificial blue light and tips for managing screen light sensitivity. All of this supports our hypothesis that people are feeling the physiological consequences of elevated screen exposure.
Why there are more screen-induced symptoms
Our devices have long been a blessing and, at times, a curse. One the one hand, technological advancements have given us greater and faster access to people, information and other resources, but it can come at a cost for our health—particularly for those with underlying sensitivities. Any increase in screen time for these individuals exposes them to greater levels of possible triggers, such as:
Screen brightness: People with migraine and post-concussion photophobia have a much lower tolerance for bright lighting from screens and other sources.1,2
Blue light from screens: Artificial blue light from our devices has been shown to have negative effects on healthy eyes and brains, let alone those with sensory sensitivities.
Sensitivity to motion: Some people with chronic illness (such as vestibular migraine or TBI) can be highly sensitive to motion, which makes animated or flashing graphics and endless scrolling potential causes for concern.
It is also important to understand the “gateway” effect that screen time can have on just about anybody’s physical health. For example, most of us have probably experienced eye strain from staring at our computer for too long; have you noticed that this sometimes leads to mild or even moderate headache pain and even sensitivity to surrounding light? And eye strain can manifest for a variety of reasons too—from difficulty in reading text on screen (which leads to a straining effect) to less frequent blinking (which can bring about dryness or irritation in the eyes).
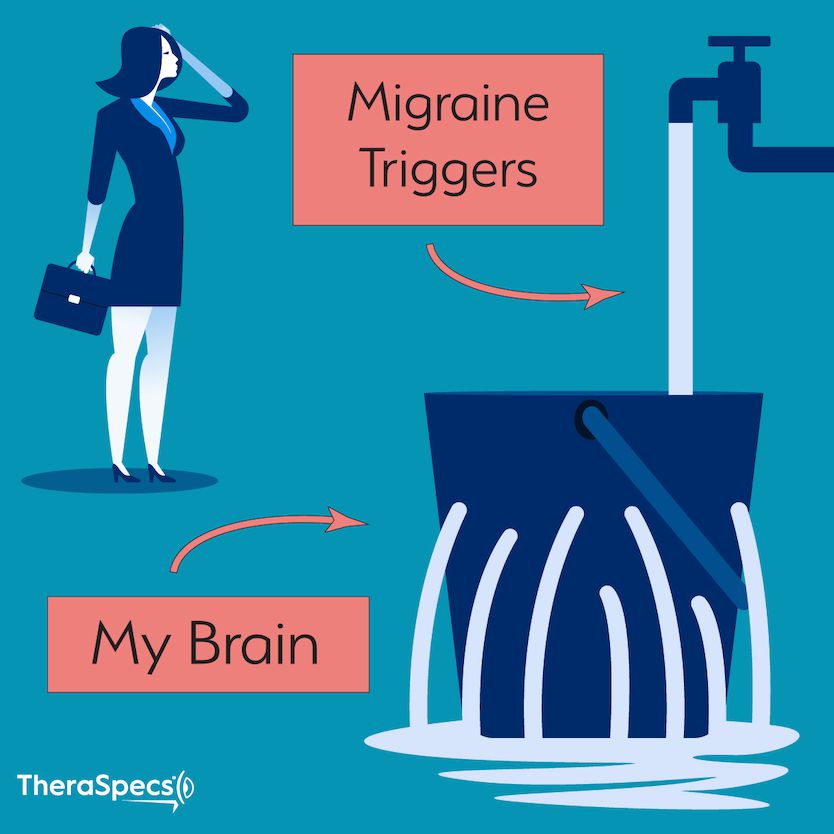
The impact can be even more pronounced if you have a neurological condition. Eileen from Migraine Strong has previously offered the concept of the Bucket Theory. This describes how triggers stack on one another, ultimately instigating a full-blown migraine attack. Some triggers you may not be able to avoid (e.g. the weather), so the bucket is never really empty. Thus, increasing your exposure to a known trigger—in this case, device screens—fills the bucket faster and can overflow more quickly into an attack unless other modifications are made.
When you compound this with other exacerbating factors unique to the COVID-19 pandemic, such as higher stress levels and less access to medication or treatment, it’s easy to see why people might be having more headaches and related symptoms during this time.
Resources to manage screen time and its effects
One thing is clear from our analysis: people are not just resigned to using their devices more without any consideration of the health consequences. 95% of all respondents to our survey have tried at least one remedy to either reduce their screen time and/or limit any negative outcomes associated with it. The most popular were:
- Wearing light-filtering glasses
- Dimming their screen
- Taking regular eye breaks
- Using dark mode or night mode
- Using blue-light filtering apps and settings
We also wanted to understand the role of our therapeutic eyewear in their screen relief toolkit, and it was clear that TheraSpecs users loved them for exactly that purpose! The overwhelming majority of those who tried multiple therapies rated our glasses as among the best or better than anything else they use to cut down on screen-induced symptoms. If you’re interested in learning more about how TheraSpecs work for screen light sensitivity, you can visit our blog article here.
Among her headache patients with rising screen time, Dr. Sheikh has made similar suggestions: "One patient is now on the computer [more] and notices more headaches, and we discussed trying to take more breaks, about every 20 minutes—and she does wear specially tinted glasses," she told us.
This reinforces the fact it often takes a proverbial “village” of therapies and behavioral modifications to effectively cut down on these complications. With that in mind, we wanted to share some additional resources to help patients better navigate the pandemic and its effects. We hope they can keep you as healthy and pain free as possible.
Screen Time Resources:
12 Hacks to Stay Headache & Migraine Free on Mobile
Computer Screens: The Effect on Headaches, Migraines & Concussion
Zoom & Migraine: Tips to Protect Users with Sensory Sensitivities
Information about COVID-19:
Latest COVID-19 Information and Guidelines (CDC)
A Chronic Illness Patient's Guide to COVID-19 (Creaky Joints)
Managing Stress, Anxiety and Depression during COVID-19 (NAMI)
Methods and Additional References:
Insights from this report were generated from data collected via:
- Google Trends, https://trends.google.com/trends/
- Google Search Console for TheraSpecs.com
- An email survey of TheraSpecs subscribers who self identify as having light sensitivity and/or being interested in light sensitivity information
- Interviews with certified headache specialists, doctors of physical therapy and neurologists
1Vanagaite J, Pareja JA, Støren O, White LR, Sand T, Stovner LJ. Light-induced discomfort and pain in migraine. Cephalalgia. 17(7), 733-741.
2Jarvis N, Starling AJ, Schwedt TJ. Photophobia symptoms and visual pain thresholds in posttraumatic headache after mild traumatic brain injury. Neurology. 2018;91(23 Supplement 1). doi:10.1212/01.wnl.0000550668.55103.10.
TheraSpecs Glasses for Light Management
Try our light-filtering glasses and stay protected against harsh light from screens, fluorescents, LEDs, unwanted blue light, bright sunlight, flashing lights, and more.





